Abstract
Familial Chylomicronemia Syndrome (FCS) is a rare autosomal recessive monogenic disease, with one to two individuals in every million, most often caused by mutations in the lipoprotein lipase gene. People affected by FCS have abnormal persistence of circulating chylomicrons following a fasting period of 12 – 14 hours, and therefore fasting concentrations of triglycerides are above 880 mg/dl. Since acute pancreatitis and cardiovascular complications can be significantly accelerated, we wish to recommend the importance of diagnostic vigilance for FCS. We also wish to emphasize the critical role of a multidisciplinary approach to such a disease; with team-work done by endocrinologists together with laboratory physicians, internists, gastroenterologists and cardiologists. Let’s make a difference for our patients!
Keywords: Familial Chylomicronemia Syndrome; Lipoprotein Lipase Deficiency; dyslipidemia; diabetes, lipoproteins.
Introduction
Diabetic dyslipidemia is usually constituted by three concomitant plasma lipid alterations: elevation in the levels of triglycerides, a reduction in high-density lipoprotein (HDL) concentrations, and the predominance of atherogenic small dense low-density lipoproteins (LDL) [Krauss 2004]. This form of dyslipidemia is known as lipid triad or as atherogenic lipoprotein phenotype [Rizzo 2005]. Hypertriglyceridemia is indeed often associated with visceral obesity, insulin resistance, type 2 diabetes and the metabolic syndrome [Dallinga-Thie 2016, Rizzo 2013]. The complications related to hypertriglyceridemia are very similar to those of other dyslipidemias, therefore we can observe an increase of cardiovascular risk on athero-thrombotic basis; in addition, it should be considered that a significant raise in triglyceride concentrations also increases the risk of liver steatosis as well as the risk of acute pancreatitis [Giglio 2021, Patti 2019].
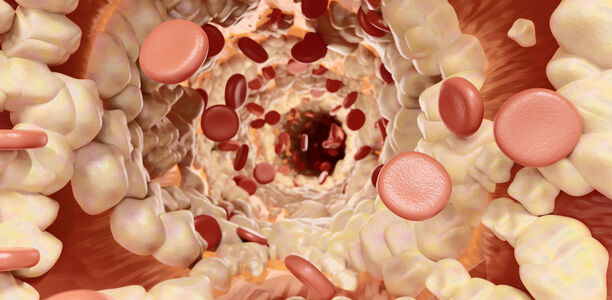
Beyond the forms of hypertriglyceridemia due to altered eating behaviours, excess alcohol consumption or specific disorders, some are predominantly based on genetic alterations [Rygiel 2018]. In the present article we will discuss hypertriglyceridemia determined by the deficiency of lipoprotein lipase, which is one of the two lipase enzymes with a key role in serum lipid metabolism. Indeed, the function of lipoprotein lipase is to hydrolyze triglycerides from chylomicrons (CM) and very low-density lipoproteins (VLDL) to produce fatty acids and glycerol, which subsequently enter the cells and can be resynthesized into triglycerides in the adipose tissue [Barylski 2014]. The other enzyme is hepatic lipase, which complements the action of lipoprotein lipase, since it hydrolyzes triglycerides in intermediate-density lipoproteins (IDL) and LDL [Rizzo 2004], thus promoting the formation of smaller more dense LDL particles [Vekic 2022].
Etiology, pathogenesis and clinic manifestations of familial chylomicronemia syndrome
Familial chylomicronemia syndrome (FCS) or type 1 hyperlipoproteinemia in the Fredrickson-Levy classification, comprises monogenetic disorders leading to significant fasting chylomicronemia. In most instances FCS is caused by lipoprotein lipase deficiency (LPLD), a rare (one to two individuals in every million) autosomal recessive monogenic disease [Brunzell 2001] caused by mutations in the lipoprotein lipase (LPL) gene [Rabacchi 2015] with abnormal persistence of circulating CM following a fasting period of 12 – 14 h [Gaudet 2015]. Fasting concentrations of triglycerides are above 880 mg/dl. The pathophysiology of FCS relies on the lack of a functional LPL protein, the key enzyme in the catabolism of CM and VLDL, after fat ingestion [Brunzell 2001]. The disease in its most severe form usually manifests itself in infancy, but diagnosis may also be delayed into adolescence or even adulthood.
The CM can accumulate in the skin or in the retinal vasculature (lipemia retinalis). However, the most important complication of FCS is severe acute pancreatitis with heightened intrapancreatic inflammatory tone, activation of proteolytic zymogens, and islet and acinar cell destruction. Recurrent pancreatitis can increase risk for diabetes mellitus due to progressive loss of islet beta-cell mass, chronic epigastric pain, or complications such as abscess formation. Other complications of FCS include eruptive cutaneous xanthomas and hepatosplenomegaly. [Whitcomb 2006, Valdivielso 2014, Pandol 2007] The IN-FOCUS study [Davidson 2017] also reported increased risk for cognitive and emotional symptoms such as difficulty concentrating ("brain fog") and long-term anxiety.
Verification of the diagnosis of familial chylomicronemia syndrome
In people with various metabolic disorders (diabetes mellitus, obesity, people with metabolic syndrome, and/or genetic conditions such as familial dyslipidemias) and severe hypertriglyceridemia (severe hypertriglyceridemia: 1 000 to 1 999 mg/dl; very severe hypertriglyceridemia > 2 000 mg/dl), the diagnoses of familial dysbetalipoproteinemia and FCS are typically not made due to the associated comorbidities. Patients are typically evaluated by multiple specialists or hospitalized for recurrent pancreatitis before they are correctly diagnosed, highlighting a lack of awareness about FCS [Berglund 2012, Tannock 2000]. People with LPLD have latescent blood serum (severe hypertriglyceridemia above 10 mmol/l in the fasting state) with a white CM layer that floats above the other plasma components after refrigerating overnight; the finding of severe hypertriglyceridemia in three consecutive samplings is suggestive of a genetic disease. In FCS it is important perform genetic screening in order to confirm the molecular diagnosis [Stroes 2017]. FCS should be considered in people with fasting triglycerides >880 mg/dl in 3 consecutive blood samples [Stroes 2017]. In addition, people with FCS often manifest with a combination of hypertriglyceridemia and hyperchylomicronemia.
FCS should be differentiated from combined polygenic hyperlipidemia (pCH). Apoprotein B100 (ApoB) is a relevant and simple biochemical parameter to differentiate FCS from pCH. People with FCS have low to normal levels of ApoB (<100 mg/dl), while patients with pCH have ApoB levels above 120 mg/dl [Stroes 2017, Pugni 2014, Sveger 2004]. Another diagnostic test is measurement of LPL activity. People with FCS have a severely reduced or undetectable level of LPL activity. It is necessary to know the medical and family history to rule out any secondary causes of polygenic hyperchylomicronemia and secondary HTG (alcoholism, obesity, insulin resistance, decompensated diabetes, metabolic syndrome, severe hypothyroidism, autoimmune diseases) [Brunzell 2001] and to identify past episodes of acute pancreatitis or frequency of idiopathic abdominal pain [Stroes 2017, Brunzell 2016]. Other causes of hypertriglyceridemia (paraproteinemic disorders, alcoholism, hormone therapy, neurological and antihypertensive agents) should be ruled out.
Pharmacologic management of familial chylomicronemia syndrome
Accurate treatment and diagnosis is key for people with FCS to receive treatment and support. The purpose of therapy is to reduce the chylomicronemia as well as its associated complications. The mainstay for management of FCS is a diet severely restricted in fat content (20 – 25 g/day), which can negatively impact quality of life [Gaudet 2010, Bruno 2010]. The fibrates and omega-3 fatty acids are only marginally effective in these patients [Valdivielso 2014].
Alipogene tiparvovec (AAV1-LPLS447X gene therapy) was the first gene therapy for patients with LPLD and severe or recurrent pancreatitis [Ylä-Herttuala 2012, Gruntman 2018] and was indicated for people whose diagnosis of LPLD has been confirmed by genetic testing. This product is, however, no longer available in Europe. Several other pharmacological agents may contribute to the successful treatment of FCS in the future [Brahm 2015]. Volanesorsen is a second-generation antisense oligonucleotide drug targeting Apo C3 messenger RNA [Rocha 2017]. Apo C3 reduces the clearance of triglyceride-rich lipoproteins from plasma by inhibiting LPL and LPL-independent mechanisms. Treatment with volanesorsen results in large reduction in triglyceride levels from baseline after 3 months [Panta 2015]. Mipomersen is another antisense mRNA compound directed against apoB mRNA that impairs the synthesis, lipidation, and secretion of Apo B, resulting in reduced CM and VLDL secretion from the small intestine and liver, respectively [Brahm 2015, Panta 2015]. Pradigastat is a new diacylglycerol acyltransferase (DGAT) 1 inhibitor that reduces triglyceride levels in people with FCS [Gaudet 2015]. Evinacumab is a fully human antibody that blocks angiopoietin-like protein 3 (ANGPTL3) [Gaudet 2017], an inhibitor of LPL.
- It is a rare autosomal recessive monogenic disease
- Affecting one to two individuals in every million
- Caused by mutations in the lipoprotein lipase gene.
- Fasting concentrations of triglycerides are above 880 mg/dl
- In a routine laboratory analysis FCS can be diagnosed by the overnight tube test:
- putting the serum sample of the patients at 4 °C
- a ring at the top of the tube indicates the presence of chylomicrons in the sample
Conclusions
The clinical and psychosocial burden of FCS reduces quality of life and limits job opportunities for people afflicted with FCS. The management strategies for treating FCS include a low-fat diet, alcohol abstinence, and the avoidance of drugs known to increase triglyceride levels. Traditional lipid-lowering therapies are virtually ineffective in people with FCS. Currently, volanesorsen is the only drug currently approved in the EU to effectively treat genetically proven FCS.
We wish to recommend the importance of diagnostic vigilance for this clinical syndrome [Ueda 2022]. A summary of FCS characteristics is shown in Figure 1. We also wish the highlight the critical role of a multisciplinary approach to such disease; indeed, although the role of endocrinologists and experts in lipid metabolism is crucial [Falko 2018], the high risk of accelerated complications in people with FCS should be managed more comprehensively with the support of other specialists such as laboratory physicians, internists, gastroenterologists and cardiologists. Let’s make a difference for our patients!
Erschienen in: Diabetes, Stoffwechsel und Herz, 2023; 32 (2) Seite 96-99